There is a less well-known but significant role of environmental factors in amplifying antibiotic resistance in India, which could increase as global warming picks up pace.
Nairobi/New Delhi, Jauary 8, 2018 – Antibiotic resistance is a serious and growing phenomenon that has emerged as one of the biggest public health concerns of the 21st century. It is an area of concern highlighted in UN Environment Frontiers Report 2017, an annual compilation of six emerging global concerns.
Antibacterial resistance (ABR) refers to the ability of bacteria to overcome the effect of antibiotics and continue to multiply. By 2050, estimates put infections resistant to antibiotics will be the leading cause of death worldwide.
With the interconnected ecosystems of humans, animals and the environment, the exchange of bacteria is continuous. The role of the environment, particularly water, in the spread of antibiotic-resistant bacteria is increasingly gaining attention.
Bacteria that have become resistant to one or all known antibiotics called superbugs, could multiply more rapidly in India because of climate change, low access to sanitation and toilets, lack of wastewater treatment, no regulations for antibiotic release in pharmaceutical wastewaters and indiscriminate use of antibiotics among the public. India is among the countries with the highest bacterial disease burden in the world, and thus the consequences of ABR could be devastating.
“We know that if there is low access to toilets, to wastewater treatment, and low hand-washing facilities, there is likely to be increased infection transmission between people. Combine this with unregulated, uninformed use of antibiotics, there could emerge a very significant problem,” William Gaze, lead author of the Frontier Report’s antimicrobial study and an expert on environment and human health, told indiaclimatedialogue.net.
Increased transmission of infections
As climate change escalates, “increased heavy rainfall and flooding can transmit infection more rapidly, both antibiotic resistant bacterial infection (from water) and person-to-person infection,” Gaze said. “On one hand, we have climate change, and on the other, an increasing global population which means more demand on the environment, more pollution and more waste to dispose off. Heavy rainfall, flooding and wastewater treatment don’t work well together; sometimes even in developed countries systems cannot cope.”
Research done by Sumanth Gandra, infectious disease physician at the Center for Disease Dynamics, Economics & Policy (CDDEP) in New Delhi has shown that during pilgrimages in India, the locations’ waste treatment capacities were overwhelmed (same as in heavy rainfall flooding) by millions of people congregating and waters bodies were found teeming with superbugs. It is not known if people were infected because this could only be known during a later infectious illness and antibiotic administration.
“Climate change can impact disease dynamics and increased use of antibiotics,” Gandra told indiaclimatedialogue.net. “Climate change-related viral infections like dengue and chikungunya (transmitted by mosquitoes), which are not bacterial infections, but because they present a fever will be administered antibiotic leading to increased anti-biotic resistant bacteria sent into wastewaters.”
“In temperatures that are getting higher, polluted waters may well see higher reproduction rates of the superbug,” Gaze said. “Since these can travel or be replaced rapidly around the globe, superbugs high growth in tropical countries poses as much risk to cooler or developed countries; their movement cannot be controlled.”
Unnecessary antibiotics use
Virus is not treatable by antibiotics, said Gaze, but it is common in developing countries to take an antibiotic for even cough and cold. The medicine has no effect on the virus; instead it increases resistance in the gut bacteria. When gut bacteria are excreted directly into the environment (through open defecation or untreated sewerage), it increases levels of antibiotic resistant bacteria in water. When this water is used for drinking, or even irrigation, the cycle is complete.
“Normal bacteria can acquire one or multiple antibiotic resistant genes very quickly even instantly in the environment,” said Gaze, “as innumerable of them compete with each other for resources.”
Bacteria can acquire resistance through a mutation in bacterial DNA or by gaining the resistance genes through horizontal gene transfer when DNA moves from one bacterium to another.
There are natural antibiotic compounds in the environmental bacteria as well, such as the bread mould from which penicillin, the first antibiotic was derived but they occur in tiny amounts. Humans now are producing hundreds of thousands of tons of antibiotics, a substantial but not yet quantified amount of which is released into the environment.
“The declining efficacy of existing antibiotics potentially jeopardises outcomes in patients undergoing live-saving surgery, organ replacement and immune-suppressing cancer chemotherapies that rely on antibiotic, which is becoming a matter of grave concern,” said Gandra.
It is estimated that 80% of the antibiotics sold by multinational pharmaceutical companies in the global market are manufactured in India and China. However, the wastewater effluents from the antibiotic manufacturing units contain a substantial amount of antibiotics, leading to contamination of rivers and lakes, Gandra says in his 2017 joint study titled Scoping Report on Antimicrobial Resistance in India.
Gaze cites a finding where a drug factory in India was found to have the same level of antibiotics in its wastewater as in the blood of a person under treatment for severe infection.
Gap in standards
In India, the existing good manufacturing practices framework (GMP of the World Health Organisation 2016) is restricted to drug safety and does not include environmental safeguards. Environmental discharges regulation is left to the local governments. Again, the Central Pollution Control Board’s effluent standards (CPCB Effluent Standards 2013) for pharmaceutical industry waste, with all state PCBs using the same standards, do not include antibiotic residues, and thus they are not monitored, according to Gandra.
“What we are seeing currently is antibiotic resistance going up, whereas new antibiotic drugs are going down. It’s got to the point now that some superbugs have no antibiotic that can treat them,” Gaze expressed concern. “Understanding how antibiotic resistance occurs, and at the same time, developing new antibiotics is very important. At the same time, environmental waste management is critical.”
“Experts are now working at finding more antibiotic products from nature. Maybe in time a completely new type of drug will be found. There are also experiments using viruses to kill bacteria,” Gaze said.
“We need to work on more vaccination for viral infections. Vaccine can prevent the disease itself and indirectly restrict antibiotic use,” Gandra said on ways to curb the superbug menace in India.
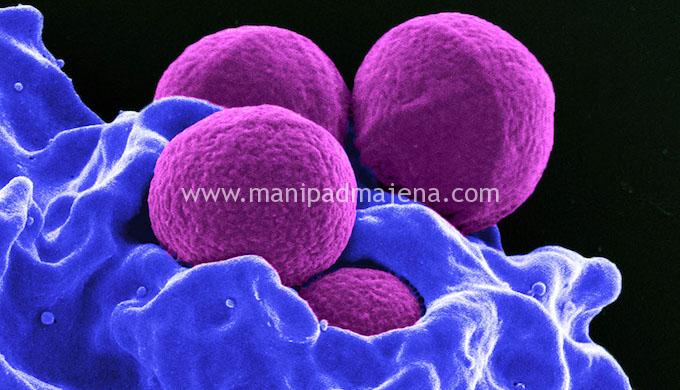
Featured Image: Methicillin-resistant Staphylococcus aureus bacteria being enveloped by a human white blood cell (Photo by US National Institute of Allergy and Infectious Diseases)
Read Original article at: India Climate Dialogue http://indiaclimatedialogue.net/2018/01/05/climate-change-amplifies-superbugs-resistance-antibiotics/